Helping Home Health Care Fulfill Its Promise to Everyone
Home health care typically brings to mind our aging loved ones. It could be a grandparent, a family friend, or an aunt or uncle after joint replacement surgery. Take a moment and think of who you know, and who has been the recipient of home medical care. For me, it was my father. He was diagnosed with Alzheimer’s disease in 2020. We were devastated but sadly not surprised. We had been concerned by recent signs that his cognitive skills were failing. For a while, he could remember a single task, like going to the kitchen to get a cookie. But if you asked him to get a cookie and a spoon, he would come back with only one of them or sometimes nothing at all. Or if you gave him one sock and asked him to put it on his left foot, he could do that. But if you gave him both socks simultaneously, he could not figure out what to do next.
The doctor informed us that there was no cure, but regular memory exercises, among other things, had a chance to slow his cognitive decline. Because my mom was a heart attack survivor and unable to drive, she could not take him to see medical professionals, so the doctor provided a referral to home health care for both of them. It seemed like a great idea, since they couldn’t go to the medical care, why not bring medical care to them? Desperate to get my mom some help and provide my dad with any possible benefit for his condition, we were very excited.
That is when our troubles began.
We called the home health agency that had been recommended and learned they were severely backed up and would not be able to accept the referral. After another week spent trading several more messages with the doctor’s office and additional referrals, we encountered the same problem with five more home health agencies. We were very frustrated, but at the same time, we thought it was probably just the disruption of the global pandemic. After all, who wanted to venture into other people’s homes at that time?
Since then, we have learned that COVID only exacerbated what you might call a “pre-existing condition” in the home health sector.
Sure this may be an interesting story, but why should it matter to you?
Let me put it in perspective next to mental health, a topic where awareness has grown greatly in the past few years. The National Institute of Health says you have a lifetime chance of developing a mental illness of 47%.
Now by comparison, if you live to be 65, you have a 70% chance of developing a severe need for long-term services or support before you die. That means explicitly home health care or nursing home care. Put more bluntly, nearly everyone will experience this story- if not later in your own life, then certainly someone you know and love. Sooner or later, you WILL be impacted.
The fact of the matter is, before COVID, and still even today, home health agencies are denying nearly half of all home health referrals across the country. Four out of every 10 people WHO DESPERATELY NEED CARE AT HOME CANNOT ACCESS IT. What happens instead is, they go without. People and their families suffer. Or those in need end up in an ambulance headed to the hospital, costing insurers and taxpayers thousands of dollars more than it would have cost to provide care at their homes.
Or, people simply die. At home. Many are in pain. While waiting for care.
So, what is causing the problem? Why isn’t there enough capacity? Well, two reasons.
You have probably heard of the baby boomer generation. This huge population bubble is getting older and is now in the age category that typically needs home health. So we are dealing with a large-scale demographic issue.
Also, we have a labor force issue. Government reimbursement rates like Medicare and Medicaid are heavily pressured. As a result, home health is an industry that doesn’t pay so well and isn’t considered “sexy.” Many people don’t care to pursue jobs in this industry. Hiring is the number 1 challenge cited by agency operators. So we have an imbalance of supply and demand - rapidly rising demand for home health care, coupled with static or shrinking supply.
However, there is still another problem.
Would you believe me if I told you that the home health industry provided 700 million home visits in 2013, the most recent year data is readily available. And that the industry drove nearly 8 BILLION -- with a B -- miles. That is further than FedEx, UPS, and DHL combined. Most likely that total is over 10 Billion miles in 2022.
Now here is the problem:
What kills me, what really drives me nuts, is that the reason why I could not get care for my dad is simply that people at those agencies didn’t know or didn’t care to use tools to work smarter. What do I mean by that? Very few of those billions of miles were driven with any kind of logistics or schedule optimization applied. So, unlike those package delivery companies I just mentioned, the home health industry is fragmented into thousands of small agencies that do not coordinate efforts and are focused on providing quality care, not innovating how they schedule their staff. So nurses and therapists are driving back and forth past each other all day long. Unbelievably inefficient! So much wasted time and energy! This is a huge part of the reason why so many home health patients cannot get the care they need!
Logistics science has been around for a while. Those home health agencies, even the little “mom and pop shops” ought to be able to grab some commercial off-the-shelf logistics software and get their schedules optimized. Or even just Google or Apple Maps. Right? It would be in their self-interest to cut mileage expenses. So what is stopping them?
The core issue is a well-known computational theory problem called the Traveling Salesperson Problem or TSP, it is considered “NP-Hard” among scholars of computational theory, meaning that it is unsolvable or could take a supercomputer an extremely long time to solve, depending on the size and scope of the problem data set. In the case of the package delivery TSP, you have a group of trucks starting from point A, the warehouse or depot, and you need to get those trucks to all of your delivery destinations for the packages on board in the shortest time possible. All you have to do is make sure the right packages are on the right trucks in the morning, and you’re good to go.
In home health care, things are a little more complicated.
Unlike package delivery companies, home care workers don’t start from a single warehouse every day, they often start and end their days from their own home, or else start at home and end at the office, and so on. This turns the problem into a Multi-Depot TSP.
On top of that, home health caregivers have a variety of specialties, such as speech therapy, occupational therapy, physical therapy, wound care, and diabetes care, to name a few. You can’t send a physical therapist to do a nursing visit, nor vice versa. So now we have a very complex mix, a multi-depot, multi-specialty TSP.
And, we’re not through yet. Some patients have a language requirement or a caregiver’s gender preference that needs to be met. And what if a patient has a cat and a caregiver is violently allergic to cats? Naturally, we can’t allow that caregiver to enter a home with cats. And, maybe some workers only work in the morning so they can pick up their children from school in the afternoon … I think you are now grasping the massive complexity of this problem. Any home health agency that tries to use Google Maps or off-the-shelf logistics software to solve their scheduling problem quickly gives up in frustration. It just won’t work.
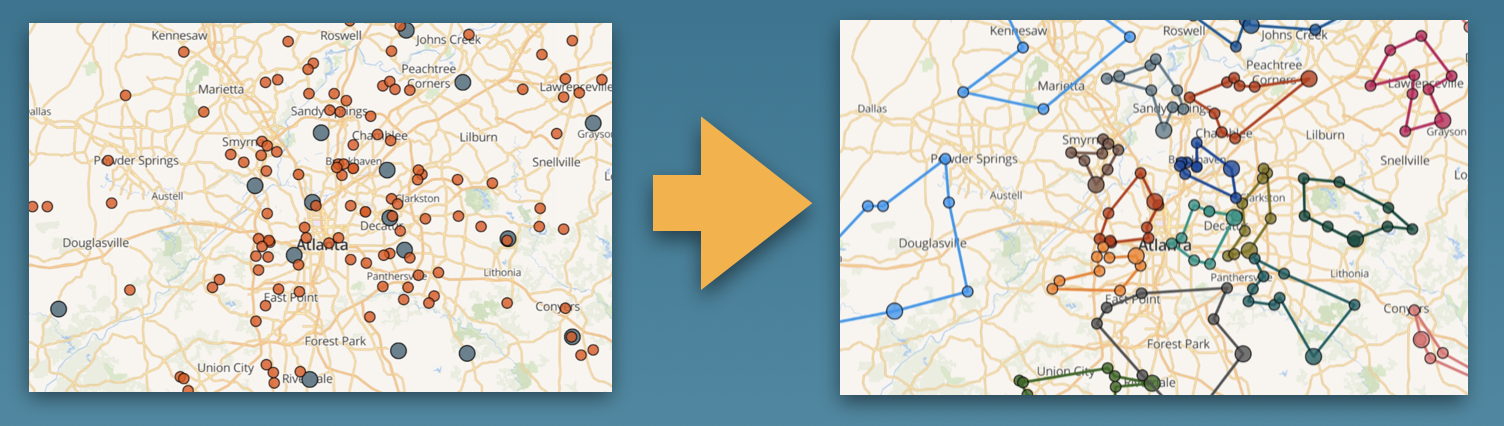
Our team set our sights on this problem long before my father’s diagnosis. It took us years of development and field testing to build a functional solution. We created an AI algorithm that models trillions of possible combinations of schedules and finds a group schedule for the entire home care agency staff and all the patients, which is highly efficient. It also takes into account all of the requirements, timeslots, and constraints that have been defined for the patients and staff.
One of our key moments was realizing that we didn’t need a 100% solution to the problem, the “one best possible” approach. That kind of model run could require days or even years. Obviously not a viable timeline for the daily fluid give-and-take of appointment setting that occurs in most home health agencies. Instead, we saw that a “95% solution” or “a really good approach” was achievable with our models in a matter of minutes. That was a vast improvement compared to the prior status quo of any agency’s scheduling.
After we solved the mathematical problem, we packaged the algorithm into a secure web application so that any customer can upload their agency data and be able to optimize their schedules within a matter of minutes.
Our early customers have been impressed with the efficiency of our software. It is so efficient that our customers typically cut their mileage and drive time in half.
But the best thing we are noticing is something else.
As we watch customers begin using the software, we are observing some other effects. And the more that we observe, the more our minds are blown by the systemic trickle-down impacts. What we are seeing goes far beyond our expectations.
With less driving time, caregivers can spend more time with patients and also get home to their families earlier. Job satisfaction increases.
Referral acceptances increase because agencies now have more capacity to take on new patients. So more patients receive care.
Agency transportation expenses decrease, allowing them to pay caregivers a higher wage to attract and retain talent.
With human scheduling effort cut by 90% and the act of scheduling turned into a single button-click, we see appointment setting democratized … imagine if I was not the nicest person when I called for care because I was worried or stressed about my dad, back then my dad might have got scheduled with a caregiver who was out of favor with the scheduling staff. With AI scheduling, all patients and all staff are treated equally and inclusively by the algorithm. Biases and human shortcomings have no role in assigning visits. No longer are schedulers able to play favorites and award preferred visits or “easy” patients to their friends. This is a huge driver of employee satisfaction and retention.
Lastly, as fuel usage drops, the carbon footprint improves, making the industry a much better steward of our planet’s resources.
There are two important takeaways I want everyone to understand after reading. First, an understanding that the accessibility of home health care will almost certainly impact everyone in this room either directly or indirectly - if not yourself when you are older, then certainly a loved one. Second, a realization that solutions do exist for the capacity and access challenges that stand in the way of people getting the care they need. The current crisis can be improved with technologies available TODAY.
In closing, I want to share one more story. In September 2021, my father celebrated his 83rd birthday. One month later, he passed away. This was the man who taught me how to fish for trout. He coached my childhood soccer team year after year. He showed me how to fix cars and houses, and how to be useful with my hands. And the most important thing he taught me? How to be a man capable of showing love. I will always carry him right here with me.
As a family, we were fortunate to have both medical insurance and long-term care insurance. However, even in our circumstances, the right care was often unavailable. There were times my mom, my brother, and I all had a share in dressing, bathing, and caring for my father. I look back on those moments as acts of love. But what if we couldn’t be there? What if my mom was having a tough day and couldn’t help at all?
Ultimately I want everyone to remember that being able to receive quality care in your own space is a basic human right. Home health care preserves our dignity and spares precious hospital beds for those who truly need them. Home health care is much more cost-effective to provide compared to non-emergency hospital visits. We, as a society, have got to do everything in our power to make home care accessible for EVERYONE, at the lowest possible cost to our environment. Only then will we ensure the well-being and dignity of ALL of us.